DENTAID EXPERTISE
News for dentistry professionals
Importance of the vestibular cortex in anterior maxillary teeth

Introduction
Post-extraction alveolar changes have been analysed in experimental (1) and clinical (2) studies and published in the literature. The vestibular cortex is the structure in the alveolar process that is most susceptible to bone remodelling after tooth extraction, and this reabsorption depends largely on the anatomy and width of the pre-existing vestibular cortex. Studying and analysing this anatomical structure is therefore of great interest to help predict the dimensional changes of the socket after extraction.
Vestibular cortex measurement methods
The vestibular cortex is a structure that is difficult to evaluate due to its reduced width and requires extremely precise and accurate measurement methods. The method of analysis of the vestibular cortex endorsed by the greatest number of scientific publications is cone-beam computed tomography (CBCT) (3). It is a non-invasive, high-resolution, low-dose radiation method that provides a complete image of the alveolar bone (4) (Figure 1).
Other methods described in the literature for measuring the vestibular cortex are probing (5) and ultrasound (6). The main objective of the analysis of the gauge of the vestibular cortex is diagnosis and planning prior to surgery, and measurement by probing is an invasive method that requires tooth extraction in order to perform the measurements (7) (Figure 2). Ultrasound has shown great potential in both the measurement of the vestibular cortex in teeth (8) and in implants (9), but to date most studies are in vitro and on cadavers, and further clinical studies would be needed to sanction its use.
Thickness of the vestibular cortex
The thickness of the vestibular cortex in the anterior maxillary teeth is scant, usually between 0.5-1 mm (10) and very often presenting some kind of bone defect. A study of the teeth in 4319 cadavers determined that only 25% presented an intact vestibular cortex (11) (Figure 3). It has also been described that in posterior teeth, including premolars and molars, this vestibular cortex is larger, on average between 1-2 mm.
There are several factors that lead us to suspect whether the vestibular cortex will be wide or narrow, even before performing CBCT. Women, patients over 50, and patients with a thin gingival biotype have shown a significantly narrower vestibular cortex in the maxillary teeth (12 – 14), just as Asian patients tend to show a narrower vestibular cortex than Europeans and Americans. Another factor that has been shown to influence the gauge of this cortex is the distance from the cementoenamel junction (CEJ) to the vestibular ridge; patients with loss of attachment who have a greater than physiological CEJ-to-ridge distance (1-3 mm) tend to present a narrower vestibular cortex.
Vestibular cortical phenotype
The vestibular cortical phenotype was classified in 2013 by Mandelaris (15) as thick when the cortex was ≥1 mm, and thin when it was <1 mm. In a prospective clinical study in 39 patients (16), a different reabsorption pattern was observed according to the phenotype of the vestibular cortex. In alveoli with a thin vestibular cortical phenotype, there was an average vertical bone loss of 7.5 mm at 8 weeks after extraction, i.e. 62% of the initial vestibular bone height. In contrast, patients with a thick phenotype showed an average vertical bone loss of only 1.1 mm or 9%. The pattern of dimensional alteration in single-tooth extraction areas with healthy surrounding dentition occurred mainly in the central area of the alveolar wall, while the proximal areas remained almost unchanged after flapless tooth extraction with 8 weeks of healing (16).
Preservation of the alveolar ridge
Ridge preservation is a guided bone regeneration technique that aims to minimise volumetric changes in hard and soft tissues after tooth extraction (17). This is a well-documented technique that shows benefits in maintaining bone ridge dimensions in comparison with spontaneous alveolar healing (18).
Although it maintains the dimensions of the alveolar ridge, the inner portion of the alveolar walls formed by fascicular bone and the thin vestibular cortices will inevitably be reabsorbed after exodontia (19). Spinato et al. (20) observed that ridge preservation in the alveoli with a thicker vestibular cortex (> 1 mm) produced a horizontal reduction of 1.29 ± 0.2 mm, while the horizontal reduction in the thinner cortical alveoli (<1 mm) was 3.22 ± 0.2 mm.
Time of implant placement depending on the vestibular cortex
Evaluation of the vestibular cortex width provides the clinician with a prognostic tool to estimate the degree of future bone loss prior to tooth extraction (21). Oral bone resorption after extraction differs between studies, individuals and location of the tooth to be extracted. Factors involved in this variation include the presence or absence of infection, flap versus flapless extraction, the degree of trauma during exodontia, and the thickness of the vestibular cortex before extraction (7).
The placement of immediate implants after extraction is a technique that decreases morbidity and shortens the time before replacing the tooth lost (22). This technique is recommended in ideal clinical conditions for a thick vestibular cortical phenotype (> 1 mm) and a thick gingival biotype (21) (Figure 4). A recent prospective study (23) of immediate implants with immediate provisionalisation showed that in the following year there was resorption of the vestibular cortex of the implant and recession of the soft tissues when the gauge of the vestibular cortex after exodontia was <0.5 mm, and that when the vestibular cortex was thicker the hard and soft tissues of the implants remained stable.
Conclusions
Analysis of the anatomy of the vestibular cortex in the anterior maxillary sector with CBCT provides the clinician with a prognostic tool to estimate the degree of future bone loss before tooth extraction. In women, those over 50, thin gingival biotypes and Asians, a narrower gauge of the vestibular cortex is to be expected, and thus the dimensional changes after exodontia will be greater.
About the Author
Julio Rojo Sanchis. Associate Professor at the University of Valencia. Member of the Spanish Society of Oral Surgery.
José Viña Almunia. Associate Professor at the University of Valencia. Member of the Spanish Society of Oral Surgery.
Bibliography
- Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005 Feb;32(2):212-8. doi: 10.1111/j.1600-051X.2005.00642.x. PMID: 15691354.
- Farmer M, Darby I. Ridge dimensional changes following single-tooth extraction in the aesthetic zone. Clin Oral Implants Res. 2014 Feb;25(2):272-7. doi: 10.1111/clr.12108. Epub 2013 Jan 25. PMID: 23346895.
- Weiss R 2nd, Read-Fuller A. Cone Beam Computed Tomography in Oral and Maxillofacial Surgery: An Evidence-Based Review. Dent J (Basel). 2019 May 2;7(2):52. doi: 10.3390/dj7020052. PMID: 31052495; PMCID: PMC6631689.
- Tian YL, Liu F, Sun HJ, Lv P, Cao YM, Yu M, Yue Y. Alveolar bone thickness around maxillary central incisors of different inclination assessed with cone-beam computed tomography. Korean J Orthod. 2015 Sep;45(5):245-52. doi: 10.4041/kjod.2015.45.5.245. Epub 2015 Sep 23. PMID: 26445719; PMCID: PMC4593869.
- Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencing ridge alterations following immediate implant placement into extraction sockets. Clin Oral Implants Res. 2010 Jan;21(1):22-9. doi: 10.1111/j.1600-0501.2009.01825.x. Epub 2009 Nov 13. PMID: 19912273.
- Glüer CC, Wu CY, Jergas M, Goldstein SA, Genant HK. Three quantitative ultrasound parameters reflect bone structure. Calcif Tissue Int. 1994 Jul;55(1):46-52. doi: 10.1007/BF00310168. PMID: 7922789.
- Huynh-Ba G, Pjetursson BE, Sanz M, Cecchinato D, Ferrus J, Lindhe J, Lang NP. Analysis of the socket bone wall dimensions in the upper maxilla in relation to immediate implant placement. Clin Oral Implants Res. 2010 Jan;21(1):37-42. doi: 10.1111/j.1600-0501.2009.01870.x. PMID: 20070745.
- Chan HL, Wang HL, Fowlkes JB, Giannobile WV, Kripfgans OD. Non-ionizing real-time ultrasonography in implant and oral surgery: A feasibility study. Clin Oral Implants Res. 2017 Mar;28(3):341-347. doi: 10.1111/clr.12805. Epub 2016 Mar 19. PMID: 26992276.
- Bohner L, Habor D, Gremse F, Tortamano P, Wolfart S, Marotti J. Accuracy of High-Frequency Ultrasound Scanner in Detecting Peri-implant Bone Defects. Ultrasound Med Biol. 2019 Mar;45(3):650-659. doi: 10.1016/j.ultrasmedbio.2018.10.030. Epub 2018 Dec 26. PMID: 30593434.
- Januário AL, Duarte WR, Barriviera M, Mesti JC, Araújo MG, Lindhe J. Dimension of the facial bone wall in the anterior maxilla: a cone-beam computed tomography study. Clin Oral Implants Res. 2011 Oct;22(10):1168-1171. doi: 10.1111/j.1600-0501.2010.02086.x. Epub 2011 Feb 15. PMID: 21320168.
- Evangelista K, Vasconcelos Kde F, Bumann A, Hirsch E, Nitka M, Silva MA. Dehiscence and fenestration in patients with Class I and Class II Division 1 malocclusion assessed with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010 Aug;138(2):133.e1-7; discussion 133-5. doi: 10.1016/j.ajodo.2010.02.021. PMID: 20691344.
- D'Silva E, Fraser D, Wang B, Barmak AB, Caton J, Tsigarida A. The association between gingival recession and buccal bone at maxillary anterior teeth. J Periodontol. 2020 Apr;91(4):484-492. doi: 10.1002/JPER.19-0375. Epub 2019 Oct 8. PMID: 31512742.
- Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, Cronin RJ Jr. Relationship between clinical periodontal biotype and labial plate thickness: an in vivo study. Int J Periodontics Restorative Dent. 2011 Jul-Aug;31(4):345-54. PMID: 21837300.
- Zekry A, Wang R, Chau AC, Lang NP. Facial alveolar bone wall width - a cone-beam computed tomography study in Asians. Clin Oral Implants Res. 2014 Feb;25(2):194-206. doi: 10.1111/clr.12096. Epub 2013 Jan 7. PMID: 23294441.
- Mandelaris GA, Vence BS, Rosenfeld AL, Forbes DP. A classification system for crestal and radicular dentoalveolar bone phenotypes. Int J Periodontics Restorative Dent. 2013 May-Jun;33(3):289-96. doi: 10.11607/prd.1787. PMID: 23593622.
- Chappuis V, Engel O, Reyes M, Shahim K, Nolte LP, Buser D. Ridge alterations post-extraction in the esthetic zone: a 3D analysis with CBCT. J Dent Res. 2013 Dec;92(12 Suppl):195S-201S. doi: 10.1177/0022034513506713. Epub 2013 Oct 24. PMID: 24158340; PMCID: PMC3860068.
- Araújo M, Linder E, Lindhe J. Effect of a xenograft on early bone formation in extraction sockets: an experimental study in dog. Clin Oral Implants Res. 2009 Jan;20(1):1-6. doi: 10.1111/j.1600-0501.2008.01606.x. PMID: 19126101.
- Avila-Ortiz G, Chambrone L, Vignoletti F. Effect of alveolar ridge preservation interventions following tooth extraction: A systematic review and meta-analysis. J Clin Periodontol. 2019 Jun;46 Suppl 21:195-223. doi: 10.1111/jcpe.13057. Erratum in: J Clin Periodontol. 2020 Jan;47(1):129. PMID: 30623987.
- Araújo MG, Silva CO, Misawa M, Sukekava F. Alveolar socket healing: what can we learn? Periodontol 2000. 2015 Jun;68(1):122-34. doi: 10.1111/prd.12082. PMID: 25867983.
- Spinato S, Galindo-Moreno P, Zaffe D, Bernardello F, Soardi CM. Is socket healing conditioned by buccal plate thickness? A clinical and histologic study 4 months after mineralized human bone allografting. Clin Oral Implants Res. 2014 Feb;25(2):e120-6. doi: 10.1111/clr.12073. Epub 2012 Nov 21. PMID: 23167308.
- Buser D, Chappuis V, Belser UC, Chen S. Implant placement post extraction in esthetic single tooth sites: when immediate, when early, when late? Periodontol 2000. 2017 Feb;73(1):84-102. doi: 10.1111/prd.12170. PMID: 28000278.
- Canellas JVDS, Medeiros PJD, Figueredo CMDS, Fischer RG, Ritto FG. Which is the best choice after tooth extraction, immediate implant placement or delayed placement with alveolar ridge preservation? A systematic review and meta-analysis. J Craniomaxillofac Surg. 2019 Nov;47(11):1793-1802. doi: 10.1016/j.jcms.2019.08.004. Epub 2019 Aug 27. PMID: 31522823.
- Yang X, Zhou T, Zhou N, Man Y. The thickness of labial bone affects the esthetics of immediate implant placement and provisionalization in the esthetic zone: A prospective cohort study. Clin Implant Dent Relat Res. 2019 Jun;21(3):482-491. doi: 10.1111/cid.12785. Epub 2019 Apr 29. PMID: 31033129.

Figure 1. CBCT of an upper central incisor in the sagittal plane where the width of the vestibular cortex can be measured. In this case we see that the root is in close contact with a vestibular cortex quite uniform in width along its entire apical-coronal dimension.
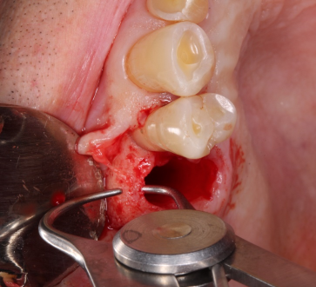
Figure 2. Measurement of the vestibular cortex after extraction of an upper premolar, lifting a flap using calipers.
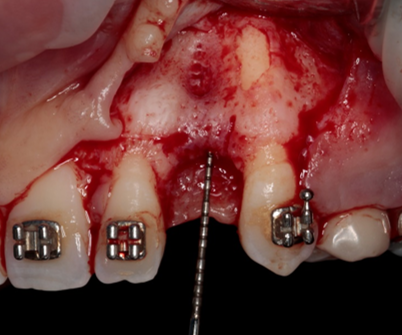
Figure 3. When lifting the full thickness of a flap in the anterior maxillary sector, 2.3 canine presents bone fenestration.
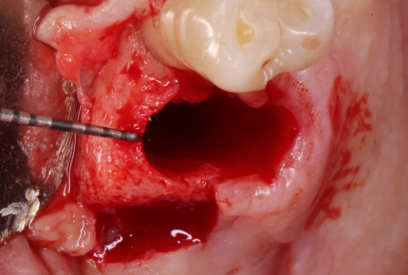
Figure 4. In a patient with a thick vestibular cortical phenotype, with a cortical width of about 2 mm, no great resorption of the alveolar ridge is to be expected, and so this would be a case for placing an immediate implant.
RELATED ARTICLES

17 Feb 2022
EuroPerio Series: professional discussions and scientific exchange
To keep the global perio community up to date with the latest research findings as well as give a taster of what is to come at EuroPerio10, the…

21 Jan 2022
Xerostomia in COVID-19 positive patients: clinical considerations
Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) the cause of the pandemic known as COVID-19, affects different organs and systems (lungs,…
20 Jan 2022
A guide adapted to Spain to optimise the approach to periodontitis
There are currently numerous clinical practice guidelines to direct the treatment of many systemic diseases (such as diabetes, depression,…
Sign up for the DENTAID Expertise newsletter
Sign up for the newsletter