DENTAID Oral Health
News for pharmacy professionals
Deciphering the role of oral health and hygiene during COVID-19
21 May 2021
The mouth is not an isolated system within the human body as a whole. The best proof of this is that there is a close relationship between periodontal diseases and several ailments including cardiovascular diseases, respiratory infections such as pneumonia and infectious exacerbations of chronic obstructive pulmonary disease (COPD), diabetes, and even adverse effects during pregnancy.
This is of particular importance at the present time, marked by the coronavirus pandemic, given the growing accumulation of evidence that highlights how periodontitis (and in general, poor oral health) can be key in the prognosis of infection by SARS-CoV-2 and could also contribute to the worsening of COVID-19.
This was highlighted in a symposium organised by the Spanish Society of Periodontology (SEPA) with the support of DENTAID at the 2nd National Multidisciplinary Congress on COVID-19. It was emphasised at this multidisciplinary forum that the mouth is a major path of entry for SARS-CoV-2 into the body, as well as being a possible source of transmission, a reservoir and an infection hotspot; For this reason, it is considered that adequately protecting the oral cavity can be essential in preventing infections and even in reducing complications in patients with COVID-19.
The three main paths of entry for the SARS-CoV-2 virus, which causes COVID-19, are through the mucous membranes of nose, mouth and eyes. During the first ten days after transmission and while the patient is asymptomatic (but highly contagious), the virus accumulates mainly in the nasal, oral and pharyngeal areas, and only later builds up in the lungs.
In the specific case of the mouth, there is currently indirect evidence that suggests how poor oral health may increase expression in the oral mucosa of what are known as ACE2 receptors, thanks to which the SARS-CoV-2 virus penetrates our cells. In fact, the existence of a significant expression of ACE2 receptors in oral mucosa, especially on the tongue, has been confirmed; furthermore, the salivary glands hold a significant number of these receptors, even greater than that in the pulmonary mucosa. Therefore, the mouth seems a very suitable place to not only receive SARS-CoV-2, but also to store it and transmit it to other people. In addition, storing the virus in the mouth as a reservoir facilitates its transmission, from person to person, through saliva droplets that an infected person may discharge when talking, coughing, sneezing, exhaling, etc.
In search of answers
Although the currently available studies are merely observational and do not allow for definitive conclusions to be drawn on the origin of this cause-effect relationship between poor oral health and COVID-19, several prospective controlled studies are being designed and performed to try to validate the main hypotheses. As Dr Miguel Carasol, a co-moderator at the symposium and the scientific coordinator of the SEPA working groups clarifies, “the biological plausibility of this link is supported by the presence of common risk factors (like smoking), and comorbidities (such as, for example, diabetes), systemic inflammation associated with periodontitis, and the existence of an altered chronic immune response in patients with periodontitis.”
According to Mariano Sanz, a professor at the School of Dentistry of the Complutense University in Madrid and a patron of the SEPA Foundation, “these hypotheses are based on many years of research into the consequences of untreated periodontitis in the development of a generalised process of systemic inflammation, and the implications of this situation in the appearance or aggravation of other pathologies, such as diabetes or atherosclerotic cardiovascular diseases.”
A recent study coordinated by Prof. Sanz shows that COVID-19 patients with periodontitis suffer greater complications, and even show a higher death rate. Specifically, it has been observed that patients with periodontitis are almost 9 times more likely to die, 4 times more likely to need assisted ventilation, and approximately 3½ times more likely to be admitted to an ICU if they have COVID-19.
It is currently understood that undiagnosed and/or untreated periodontitis poses a risk of aggravating the systemic condition of patients with COVID-19, especially in more severe cases, and more so in patients admitted to ICUs under assisted ventilation. Aspiration of periodontal pathogens into the bronchial tree and the inflammatory response typical of periodontitis may justify this aggravation, which is still associated with a higher risk in patients with diabetes mellitus or those who are obese or suffering from previous respiratory disease, since periodontitis can affect the evolution of these conditions.
Periodontitis, obesity, diabetes and COVID-19
Thus, for example, periodontitis and obesity are common comorbidities associated with systemic inflammation; therefore, when they coincide, their damaging effects on other organs and systems are enhanced. For Dr Francisco Tinahones, head of the Endocrinology and Nutrition Service of the Virgen de la Victoria Hospital in Malaga and chair of the Spanish Society for the Study of Obesity (SEEDO), “the role of obesity is crucial in the occurrence, severity and mortality due to COVID-19.”
On the other hand, the inflammatory state that accompanies diabetes is associated with an increased risk of complications from COVID-19, especially those related to a phenomenon known as “cytokine storm”. In some of their tissues, including the lungs, diabetics present an altered expression of the ACE2 protein, the SARS-CoV-2 receptor, and increased angiotensin 2, which would make them more susceptible to COVID- 19. Furthermore, hyperglycaemia is associated with impaired innate and adaptive immunity, which also contributes to the severity of SARS-CoV-2 infection in diabetics. Other factors inducing a more severe form of COVID-19 in diabetics include: coexistence of obesity in type 2 diabetics; endothelial inflammation induced by SARS-CoV-2 infection (which aggravates the endothelial dysfunction observed in the diabetes) and hyper-coagulation in COVID-19 infections, which increases the thrombotic tendency in diabetes.
As the specialist in Endocrinology and Nutrition and the coordinator of the SEPA-SED Working Group Dr Juan Girbés explains, “all this makes it more likely for people with diabetes to present symptoms and to have more serious symptoms of COVID-19, which is what has been observed in clinical practice.”
This evidence combines with the accepted bidirectional relationship that exists between diabetes and periodontal disease: it is acknowledged that people with diabetes not only have a greater risk of developing periodontitis and that this occurs more aggressively, but the fact of having a chronic infection such as periodontitis also makes glycaemic control difficult in diabetics, increasing the risk of complications. Both diabetes and periodontitis are accompanied by a situation of underlying chronic inflammation, they share mediators, and are associated with an increased risk of cardiovascular complications.
Periodontitis occurs with low-grade systemic inflammation and high levels of cytokines. “Epidemiological, experimental and intervention studies have shown that periodontitis can also affect systemic health, and periodontitis has in fact been independently associated with diabetes, cardiovascular disease and even premature mortality,” says Dr Girbés.
Thus, and as stated by Dr Eduardo Montero, an associate professor of Dentistry at the Complutense University in Madrid, “assuming that periodontitis contributes to low-grade systemic inflammation and that COVID-19 infection gives rise to an acute systemic inflammatory response, it may be concluded that periodontitis could ‘amplify’ the inflammatory response in patients with COVID-19, increasing the risk of complications in these patients.”
Relationship between periodontitis and lung infection
Before the SARS-CoV-2 pandemic, associations had already been established between lung infections and periodontitis with high levels of periodontal pathogens, and in general with poor oral hygiene. To explain this relationship, especially in long-term or ICU patients, we need to turn to the role that aspiration of bacteria from the mouth may have, considering that in patients with periodontitis there are higher amounts of biofilm and more pathogenic bacteria, which is especially relevant in the context of COVID-19.
“The relationship and influence that periodontitis has on the occurrence of bacterial pneumonia has been demonstrated,” says Dr Jordi Almirall, an intensive medicine specialist and member of SEPA and the Spanish Society of Pulmonology and Thoracic Surgery (SEPAR). In the specific case of COVID-19, which is a viral disease, it is accepted that it can by itself cause viral pneumonia, but it can also act as a predecessor of bacterial superinfection by organisms residing in the oral cavity. Based on experience and on population-based case-control studies, it has been shown that periodontitis favours the occurrence of community-acquired pneumonia and that “this is possibly so because periodontitis favours colonisation and/or virulence of microorganisms that act as pulmonary pathogens.” In this regard, Dr Almirall recommends that “COVID-19 positives maintain good oral hygiene to reduce the bacterial load that can be aspirated to the extent possible.”
According to Blanca Paniagua, an associate professor in the Degree in Dentistry and Master of Periodontology and Implant programmes at the International University of Catalonia (UIC), “the link between periodontitis and respiratory disease is more evident in debilitated older adults, hospitalised patients with functional dependence for eating and oral care, and patients with dysphagia, considering this as the most fragile and vulnerable population group to suffer aspiration of the oral content into the lung.”
Based on these facts, Dr Paniagua recommends that “in patients with COVID-19, and especially in those who are hospitalised for this disease and/or who require mechanical ventilation, all measures aimed at maintaining good oral hygiene and reducing bacterial plaque build-up should be taken in order to prevent or minimise the risk of aspiration of pathogens.”
Proven benefits of optimum oral hygiene
In this regard, Dr David de la Rosa, the chair of the Scientific Committee of the 2nd National Congress on COVID-19, highlights the importance of always maintaining good oral health in order to care for overall health. “Improving preventive oral hygiene measures and treating periodontal disease can be associated with a decrease in the risk of developing pneumonia, exacerbation of COPD or other viral diseases, as well as their severity. It is therefore highly important to perform oral health prevention campaigns, especially for people at risk, including adequate prevention and/or treatment of periodontal disease.”
As the experts from the different dental and medical disciplines gathered at this symposium have shown, it is especially crucial at this time to keep good oral health, because it can help prevent the development of infectious diseases like COVID-19. Therefore, they highlight the importance of good oral hygiene as a preventive measure and point to the need to include it in the package of basic preventive measures currently recommended, along with hand washing and social distancing.
In addition, the results of the latest laboratory studies show that some mouthwashes inactivate the SARS-CoV-2 virus, suggesting that they could reduce the viral load and the risk of transmission of the virus, reinforcing the important role that the mouth would play in the pandemic. As indicated by Prof. David Herrera, a patron of the SEPA Foundation and a co-director of the ETEP Research Group (Aetiology and Therapeutics of Periodontal and Peri-implant Diseases) at the Complutense University in Madrid, “it is believed that the use of virucidal mouthwashes could reduce the risk of transmission by infected individuals and also reduce the risk of developing more severe COVID-19.”
Numerous studies have analysed the efficacy of certain mouthwashes widely used in dentistry to reduce viral load, and thus prevent infection by the SARS-CoV-2 virus. Of all of these, the compounds formulated with antiseptics such as cetylpyridinium chloride (CPC) or povidone iodine, have shown the clearest results in in vitro studies, and are currently being clinically evaluated.
Even without these findings being as yet replicated in clinical trials, it is clear that the use of these mouthwashes in the dental clinic before performing certain dental treatments is highly advantageous. Furthermore, as Dr David Herrera points out, “they are probably useful in patients with COVID-19, close contacts or in patients at risk, and their preventive capacity should be studied in greater detail when they are used by the general population.”
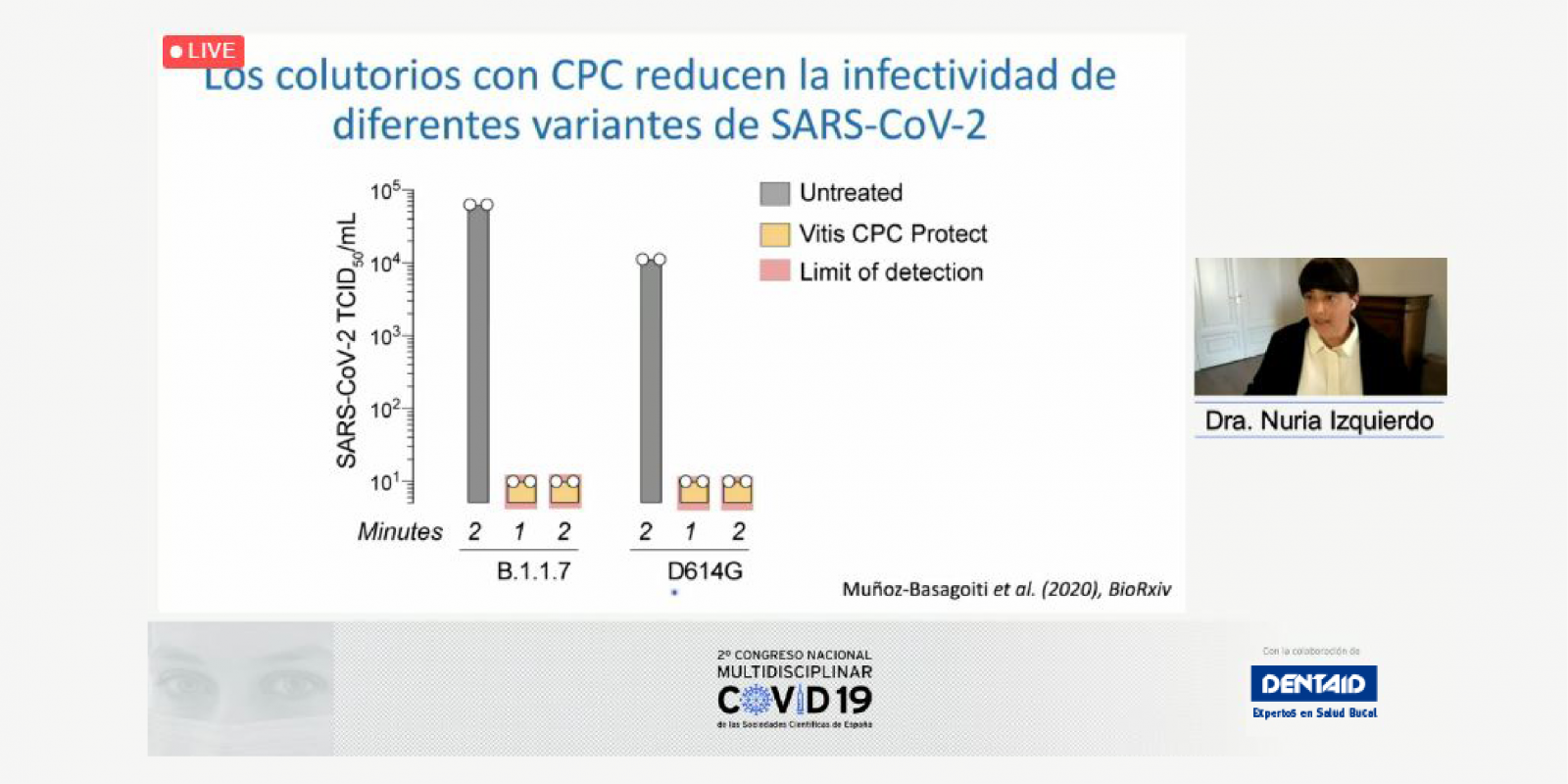
In the case of mouthwashes with CPC, “these inhibit the entry of the SARS-CoV-2 virus into susceptible cells and are effective against different variants of the coronavirus. They act by disrupting the SARS-CoV-2 membrane, and it has been shown in in vitro laboratory studies that they reduce the infectivity of SARS-CoV-2 by 1000,” explains Nuria Izquierdo-Useros, the lead researcher of the Pathogen Immunity, Signalling & Therapeutic Applications (PISTA) group at IrsiCaixa in Badalona, near Barcelona. Her research group is currently “evaluating whether mouthwashes with CPC reduce the viral load in the saliva of those infected with SARS-CoV-2.” The aim is to determine whether it is possible to reduce the transmission of the virus and prevent new infections by reducing the viral load in the saliva of infected persons.
RELATED ARTICLES

07 Oct 2021
Warding off the smoke from the dental clinic
Kicking the smoking habit is the best thing a smoker can do for their present and future health, gaining in quantity and quality of life. The task is…
12 Apr 2021
10 things you need to know about diabetes and periodontitis
It has been found in recent years that the link between periodontitis and diabetes is bidirectional. While diabetes increases the risk of periodontal…

03 Oct 2019
CONSENSUS AND MULTIDISCIPLINARY VIEW OF THE MANAGEMENT OF ANTI-THROMBOTIC TREATMENT
The Spanish Society of Periodontology (SEPA) is one of the scientific societies that has participated in the elaboration of a consensus document of…
Sign up for the DENTAID Oral Health newsletter
Sign up for the newsletter